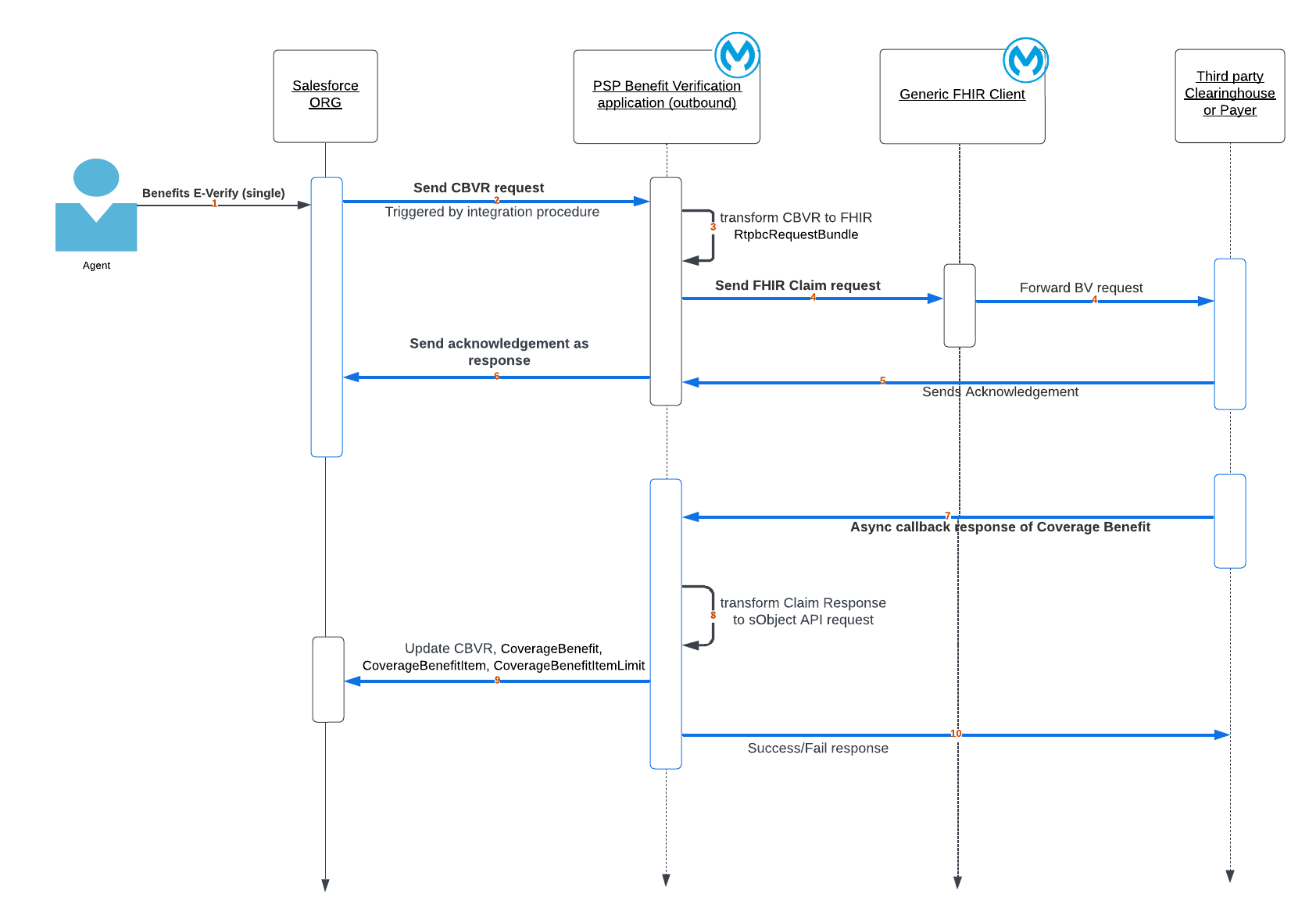
| 1 | The benefit E-verify request (Care Benefit Verification Request) is triggered by a patient services representative in the Pharma org. |
| 2 | The request is received by the Mulesoft benefit verification application. |
| 3 | The benefit verification request is transformed to an FHIR CARIN Rtpbc RequestBundle. |
| 4 | The request is sent to the clearinghouse (CH) or payer system via a generic FHIR client. |
| 5 | The clearinghouse or payer processes the request asynchronously and sends a request received acknowledgment as a response. |
| 6 | The application sends back the request received acknowledgment. |
| 7 | The third-party clearinghouse or payer sends an FHIR CARIN Rtpbc ClaimResponse for the pharmacy benefit verification request. |
| 8 | The application transforms the response to update data in the Salesforce org via an sObject API call. |
| 9 | The application updates the Coverage Benefit information in the Salesforce org. |
| 10 | The application returns a success or error response to the clearinghouse or payer. |